Primary Care NICU Nurses
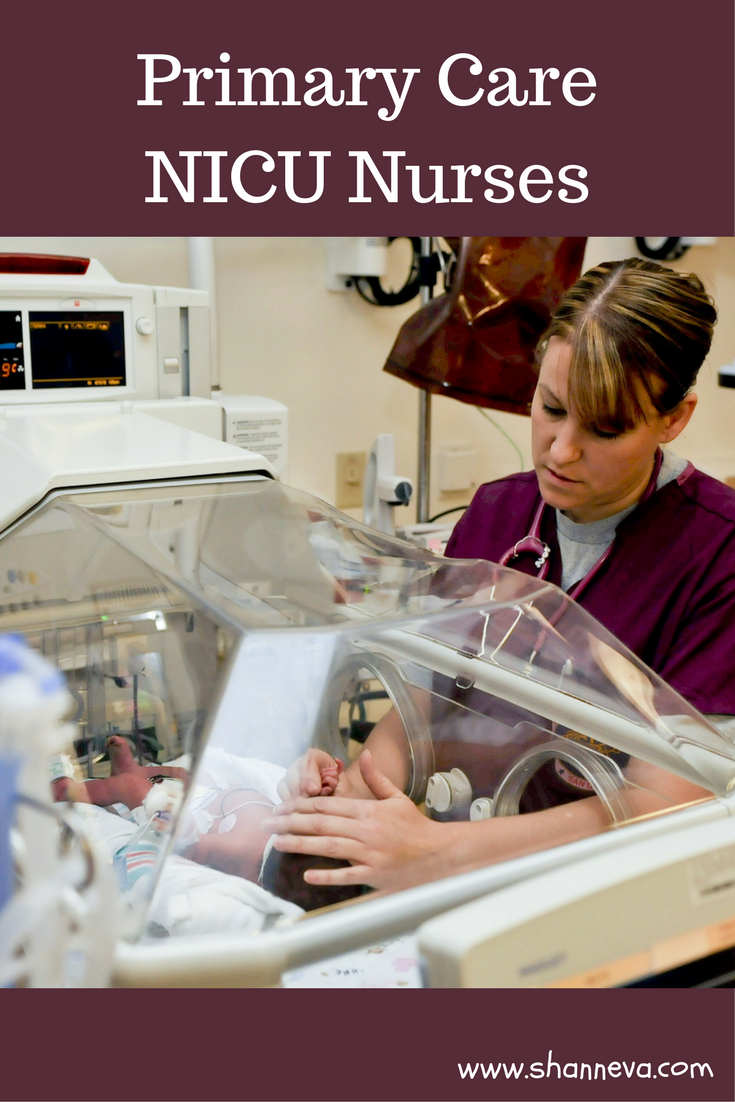
Some of the most important people in your preemies new life are their primary care NICU nurses. They are the nurses that spend the most time with your baby, and work closely with the doctors to give your baby the best care.
In our case, each of our twins had different primary care NICU nurses. I could count on them to explain to me what was happening each day, and what they were watching for. They showed me how to care for my babies, when I was afraid to even touch them because they were so tiny and fragile.
When I couldn’t be there, I knew they were in the best hands. Someone that would notice if something was wrong, someone who would advocate for them, and someone who truly cared for them.
With a two-year-old at home, I couldn’t be at the hospital all the time. I felt lucky and blessed to have nurses that were with them when I couldn’t be.
Primary care NICU nurses, and really all NICU nurses, are amazing people. They care for the smallest, sickest babies, and also for the families that are struggling in this new, intense situation. I don’t think I could ever do their job, but I’m so grateful for them.
Today’s micro preemie family shares my appreciation for primary care NICU nurses. Their 23 weeker was cared for by veterans of the NICU, and they were just so grateful.
I’m grateful to be sharing sweet Samuel’s story with you today, as told by his mom, Emily.
1. Tell us about your baby
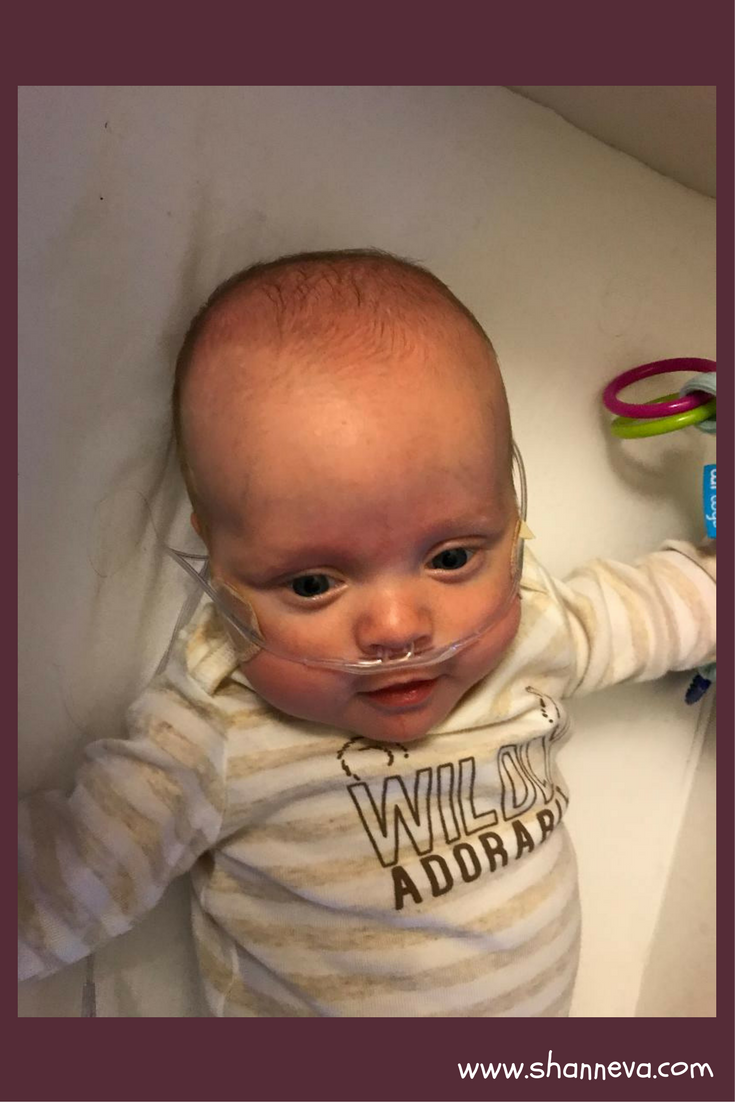
Our son, Samuel Seppo, is our first living child. He was born at 23 weeks 1 day gestation. He weighed 1 pound, 4 ounces at birth.
Sam is currently one month adjusted and he weighs eleven pounds.
He was discharged from the hospital three days after his due date, and he’s thriving at home.

2. How long was your NICU stay?
What was the hardest part?
The hardest part was not knowing what was going to happen. Everyone kept telling us that having a micro preemie in the NICU would be a rollercoaster ride, but we didn’t know what that meant. Sam had a week-long “honeymoon” at the beginning, so it was a rude awakening when he started to really struggle with breathing. I felt like I was underwater, and I spent the first two months terrified. I would have really benefited from a sit-down with a neonatologist to discuss possible complications, including their likelihood and the chances of death associated with each one. I know every baby is different and no one knew what was going to happen, but having statistics would have helped me feel like I could anticipate the possibilities and prepare for them. I would have also liked a list of things that, in the grand scheme of things, are most important. I tried to take my cues from the nurses; if they weren’t worried, I tried to learn to relax. Over time, I became much more comfortable with certain things, like apnea and bradycardia spells.
Despite my anxiety, Sam had a pretty smooth course.

Learning to Breathe
A week after birth, he was diagnosed with pulmonary interstitial emphysema (PIE), and he was at 100% O2 and still having some desats. They put him on the jet ventilator for a few days, but he didn’t tolerate it well, so he went back to the conventional jet.
At 9 days old, they gave him his first 3-day burst of decadron. They wanted to wait until he was at least two weeks old, but he needed it sooner. He really turned a corner after that.
Altogether, Sam spent seven weeks on the ventilator, five weeks on bubble CPAP, and four weeks on high flow. He’s still on low flow at home, ½ liter. It took him three tries to get off the ventilator, and two to get off of CPAP.
He had three 3-day decadron bursts, 3 blood transfusions, and he’s been diagnosed with chronic lung disease.
At 32 weeks gestation he was diagnosed with stage 2, zone 1 ROP, but it resolved by 40 weeks, and he only needs a follow-up at one year.

Complications
I almost forgot, Sam also had brain bleeds. His initial ultrasound showed a grade 1 and a grade 4 bleed. I was upset to learn that, but my fears regarding those results were eclipsed when he started having a lot more difficulty breathing that afternoon. At that point, his lungs were all I cared about. If they could have transplanted my own lungs into his tiny body, I would have jumped at the chance. Subsequent head ultrasounds brought happy news. After having several radiologists review the results and reassess the first ultrasound images, they retracted the grade 4 brain bleed diagnosis. They downgraded it to a grade 2. Our neonatologist said we could cry happy tears about it, and that she hadn’t seen such a thing happen in 18 years.
Amazing Primaries
I first held Sam at 12 days old, right after he went back onto the conventional vent and his umbilical line came out. It was Mother’s Day. I worried that the nurses were rushing to get me to hold him because of Mother’s Day, and I wondered if he was truly ready. He did great, though. We did kangaroo care as often as we could after that. Our primary nurses were fantastic and worked hard to give us many special moments with our baby. One day when Sam was a couple of months old, one of our primaries dressed him and wrapped him up in a blanket so that I could hold him in my arms and look at his face.
Speaking of primaries, we were so lucky to get two primaries who had worked in the NICU for 36 years and had a lot of experience with micro preemies. They really put my husband and me at ease. They were wonderful and we love them dearly. One of the most difficult adjustments to make while we were at the hospital was when we moved out of the NICU and into the ICC. I missed our primaries so much, I cried for a week.
3. Do you know what caused your premature birth?
My husband and I have a history of pregnancy loss, and I have had three D&Cs for babies lost at 15+3 and 12+2 weeks in 2015 and 2016. Laminaria was used to gently dilate my cervix during the 15-week loss. I was very concerned about the impact my reproductive history would have on my subsequent pregnancies, so when I was pregnant with my son, I requested that my OB perform a cervical check at 14 to 16 weeks. She was very dismissive of my concerns and she refused to do the exam, saying that my history did not increase my risk of cervical incompetence.
I wish I would have gotten a second opinion.
The First Sign
Due to my age, 35, I qualified for a level II anatomy scan without any indication of a problem. I traveled to a perinatologist office three hours away when I was 20 weeks exactly. Unlike in my previous pregnancies, our baby boy was healthy and thriving! We were so excited! Finally, we’d have a baby in our arms in just a few short months! At the beginning of the scan, my cervix was long and firm. But by the end of the exam, it was funneling and had shortened considerably. The perinatologist came in and said my cervix was dynamic and she diagnosed cervical incompetence. She gave me a shot of progesterone and prescribed progesterone suppositories to be used every night. She sent me back to my OB to have a cerclage placed the next day, and she told me not to sit upright or do anything until then.
The Procedure
The next day, my husband brought me to the hospital. The OB came in and read off the list of risks associated with the placement of the cerclage. Infection, rupture of membranes, premature delivery…I already knew these risks going in, but hearing her say them made me cry until they put me under. I begged them to keep our baby safe. When I woke up from surgery, my husband told me that the OB had spoken with him and that everything had gone wonderfully. I had 2 to 2.5 cm of cervix – the OB told him she wouldn’t have even placed the cerclage if she’d known I had so much cervix left. At our follow-up visit a few days later, the OB said that other than avoiding long-distance road trips (far from NICUs) and not having sex, I should behave normally. She did not consider me high risk, and said there was no evidence that bed rest would help anything. She didn’t want to do any follow-up visits until 28 weeks. That didn’t sit well with me, so I begged for cervical checks at 24 and 26 weeks, which she reluctantly agreed to (she explained that we were already doing everything we could, and extra exams wouldn’t cause any change in our treatment plan – I reminded her that we might want to start steroids and magnesium if it looked like delivery were imminent).
I never made it to that 24-week check.

Changes
At 22+4 I started noticing an increase in discharge. I wrote it off as normal, a result of having the cerclage. The next day I noticed a tightening of my uterus whenever I stood up. They were brief and painless, so I thought they were Braxton Hicks. That evening I had a sudden lower back ache.
I called the L&D department at my hospital, and they had me speak with a nurse practitioner. I explained my symptoms, and she told me that they were typical pregnancy symptoms, nothing to be worried about. She even checked with a doctor, then recommended that I take some Tylenol and go to sleep. I tried to be reassured by her words and I and went to sleep, but when I woke up at 3 am with menstrual-like cramps, I knew without a doubt that something was wrong.
I drove to the hospital and was admitted right away. I was 22+6. They checked my cervix and said that it was closed, but the amniotic fluid test came back positive. My membranes had ruptured. The hospital I was at did not even have a NICU, and the other hospital in town only had a level II NICU. They didn’t even try to save babies until they were at least 24 weeks.
Be Your Own Advocate
The team taking care of me all wore sad expressions on their faces, and someone brought in a little open-air cot to put the baby in once he was delivered (as if I would let him die in a little cot instead of in my arms). They gave me steroid shots and started an IV to administer magnesium, but they prepared me for the likelihood that our baby would soon be dead. Because of my previous losses, I have participated in pregnancy loss forums online. Through those forums, I have heard many stories of distressing pregnancies. One story was of a woman who had ruptured membranes at 14 weeks, but delivered a living baby at 28 weeks. So I knew it was at least possible, although certainly not guaranteed, to hold off labor for a while. I begged my doctor for an intervention, so she decided to call around to other hospitals in my state. Half an hour later she came in smiling, “Abbott Mother Baby Center will take you. They do amazing things with 23-weekers.”
There was a snow storm that day, May 1st, so helicopters were grounded, but an airplane was finally able to fly from another city to pick me up and bring me to the hospital that would save my baby. We held off labor for 44 hours from when the first steroid shot was administered, only four hours short of the 48-hour goal. My cerclage popped while I was throwing up the evening before I delivered, and our baby was born at 2:11 am on May 3rd, kicking and screaming. The pathology report on his placenta came back positive for an infection, so we feel fortunate that he came when he did before the infection passed to him.

4. How are you and your baby doing now?
Our family is doing great! It’s been an adjustment to come home. To say I was anxious bringing our baby home on oxygen would be an understatement. The first week was rough, and I thought I’d never sleep again after we had a few equipment errors. We’ve worked out the kinks now, and things are going smoothly. We anticipate having him on oxygen through the winter, as his pulmonologist is hesitant to discontinue it during flu season. He still does need the oxygen, so they wouldn’t remove it outright anyways.
Isolation
We’re doing isolation through the winter, so it’s been stressful when some of our extended family members haven’t been supportive of that decision. I naturally avoid conflict and am rather meek about saying things that have the potential to make people upset, so I suppose this is the perfect opportunity for me to learn to be more assertive. My husband and I have also adjusted our work schedules so that we can keep Sam home for his first two years.
Milestones
Our baby is doing great with milestones, although he’s still very young so it’s hard to tell. He loves to eat and he’s gaining weight steadily. We’re working on breastfeeding, although it’s somewhat difficult since I go to work and my husband stays home right now. A nurse comes out a couple of times to week to check on Sam, and we’ll start receiving visits from the Help Me Grow – Birth to Three program in a couple of weeks. We have follow-up appointments with a pulmonologist, and we’ll be sure to bring Sam to the NICU follow-up clinic. We can’t wait to see the doctors and nurses who saved Sam’s life again.
Support and Hope
This experience has had profound impacts on me and my husband. It was amazing to watch our 23-weeker bloom and develop. I didn’t even know a baby could be viable at 23 weeks! Science and technology are amazing, and the nurses and doctors even more so. We experienced a huge outpouring of support while our baby was in the hospital, both from loved ones and complete strangers. During a time of such political divisions and perpetual bad news, experiencing such kindness helped to restore my faith in fellow human beings. I am now driven to give back whenever I can. I can’t wait to go back and serve meals at Ronald McDonald House, and I’m interested in volunteering for the hospital.

5. What advice would you give to a new preemie family?
It’s hard to give advice because it’s such a stressful situation to have a newborn micro preemie. It’s not something anyone plans for or wants to have happen. It’s traumatizing. People are going to handle it however they can, and they can’t be expected to follow advice. I found it irritating when people kept telling me that I needed to take care of myself. What does that even mean when you’re fearing for your child’s life? Eating and sleeping will happen. It helps when others supply the food and bedding (and thanks to Ronald McDonald House for doing just that). Pumping, if the mother chooses, can easily take over the whole day (and night). A lot of people encouraged us to get out of the hospital and go on a date, take a walk, clear our heads. It’s stressful when people push you to do things you’re not ready for. Yes, it might help to get out of the hospital for a moment. But it’ll happen on its own when you feel comfortable enough to leave. When you fear that any moment might be your child’s last, you don’t want to miss a single one. So don’t feel bad if you don’t follow anyone’s advice!
When Sam was born, people said, “congratulations!” It felt like a slap in the face. This was a tragedy. He was supposed to be born at the very end of August, not the beginning of May! I felt like we tentatively had a child, until further notice. But over time I realized, we DID have a child, living and (kinda) breathing, and there was nothing tentative about it. Even if he died, he was our son. I tried to make the most of our time together, and I did whatever I could to make him more comfortable and let him know that I loved him.
Information Available
Once you have your mind wrapped around your new reality and hopefully feel like you can breathe a little, I guess I do have a bit of advice. Make use of your social worker and apply for all of the programs available. Our baby qualified for SSI while he was in the hospital, and Medicaid for his first year. Now that we’re home, we’ve been approved for WIC despite exceeding the income limits. We almost didn’t apply for it. It really helps, and it frees up mental energy so that we can focus on our son. Another thing I would suggest is to take a lot of photographs and video. It’s easy to forget how small they were! I took a lot of pictures with my iPhone, even though I had a nicer camera available. Now I wish I’d brought out the nice camera a little more often because the low-light conditions meant that a lot of my iPhone photos are grainy. There’s a great website that has a great list of photos you might want to take during your baby’s hospital stay: http://www.preemiebabies101.com/professional-insight-photographing-your-preemie/
I’m not sure if people at risk of going into preterm labor read this blog, but for them I would say – make a plan in case you do deliver your baby early. The hospital your baby is born at can make a huge difference in survival rates for micro preemies. Find a level three or four NICU, and maybe even give them a call. A lot of hospitals have a phone number you can call to find out survival and complication rates. Also, advocate for yourself, trust your gut, don’t be afraid of seeming overly anxious or paranoid to your partner or health care provider, and educate yourself on the signs and symptoms of preterm labor, PPROM, and infection. The cost of getting checked out at L&D when it might be a false alarm is much, MUCH lower than the $52,000 our insurance was charged to fly me to a better hospital! If I’d known better, I could have driven myself there the night before.
Thank you so much to Emily for sharing Sam, and for her great advice. He is amazing, and I’m so glad you were such a strong advocate for yourself and your baby.
Please leave any supportive comments or questions below.


It makes me so angry when doctors dismiss things. Moms know their bodies! Sweet Sam! What a little trooper! Sending them lots of hugs! Thanks for sharing this story!
Thank you for sharing your story and your sweet Sam. I’m glad he is home and doing well. NICU nurses are truly amazing. My friend who had a micro preemie still goes back and visits all her nurses and they have a cake on her daughter’s birthday each year. <3
Wow, what a strong little guy and these nurses are so amazing for not only caring for these baby’s but making the mom’s feel at little bit at ease!
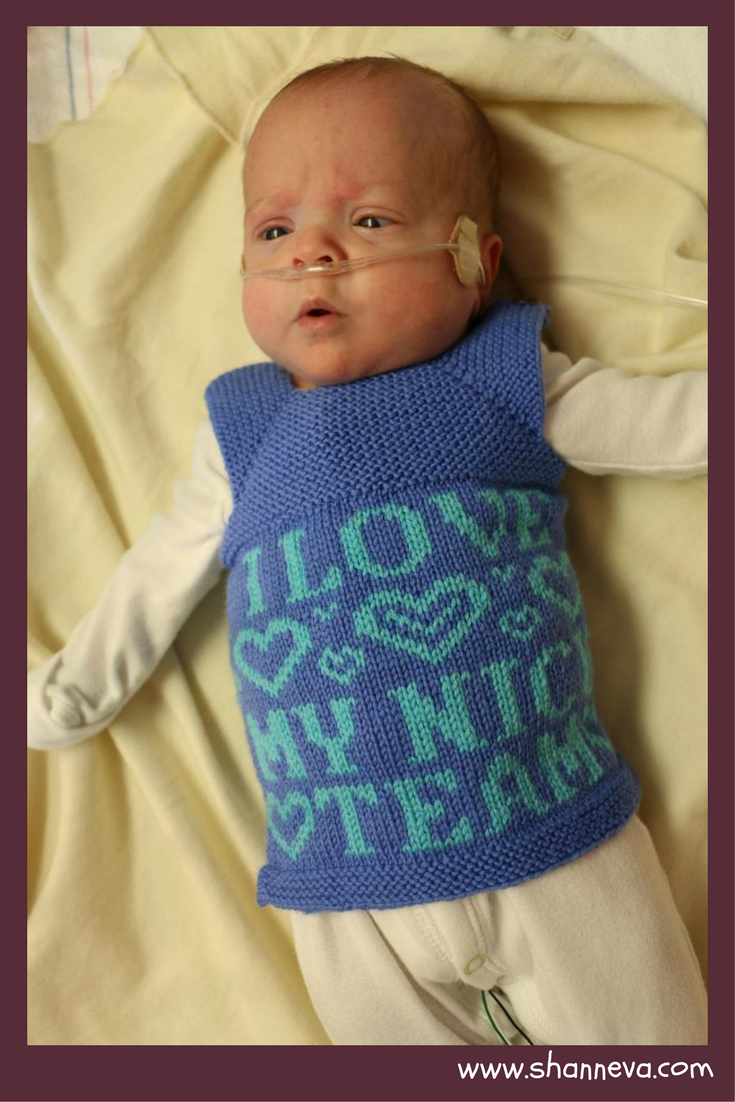
Thank you for sharing you and Sam’s amazing story Emily! What an incredible journey! I love that picture of Sam in his special little knit vest, so sweet.
I can’t even imagine the roller coaster of emotions that goes through a parent’s head during a difficult time like this. And thank god for those caring nurses, who are voices of reason and strength and compassion when parents need it the most, eh? Thank you so much for sharing this story, Shann, and for sharing all these incredible preemies here. XOXO
Thank YOU for reading them!
What an incredible story!